Lame Excuse: Rubio Cuts Off Funding to the United Nations Population Fund (UNFPA)

International family planning and reproductive health (FP/RH) advocates in Washington are perhaps unique—relative to our colleagues in other health and development sectors—in our ability to furnish to legislators and executive branch policymakers a defensible, evidence-based estimate of the appropriate U.S. government (USG) share of the cost of addressing the critical global problem we seek to solve. In our case, the motivating goal is meeting the unmet need for modern contraception of 214 million women in developing countries. The dollar amount proposed each year by FP/RH advocates to achieve this ambitious goal is widely accepted. It has been referenced in the budget and appropriations recommendations made by members of the House and Senate and incorporated by several foreign assistance coalitions as part of their own funding “asks.” However, the detailed methodology used in this calculation has been less well-documented publicly—until now—and is thus explained.
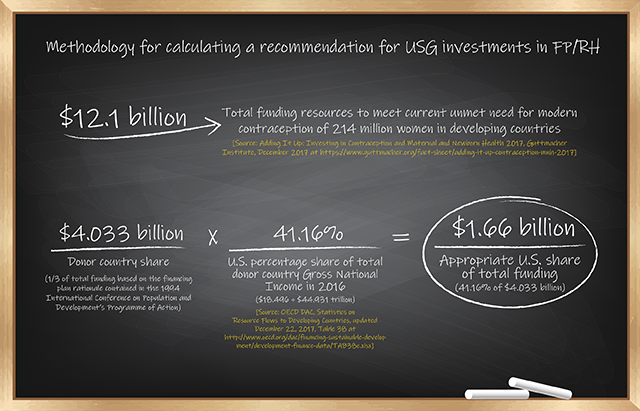
The calculation of the U.S. share of the total funding resources required to meet the current unmet need for modern contraception of women in developing countries is derived from a methodologically rigorous analysis done by the Guttmacher Institute called Adding It Up: Investing in Contraception and Maternal and Newborn Health. According to the December 2017 analysis, satisfying the current unmet need for modern contraception of 214 million women of reproductive age in developing countries who want to avoid pregnancy but are not using a modern contraceptive method would cost a total of $12.1 billion annually.
Working from the global contraceptive cost calculation of $12.1 billion, how are relative shares of the financial burden assigned among donor nations and recipient countries in the developing world? At the 1994 International Conference on Population and Development (ICPD) in Cairo, 179 United Nations (UN) member states agreed by consensus—purportedly for the first time during an international conference—on a costed implementation plan designed to achieve the goal of significantly expanding access to reproductive health care, including family planning, through 2015. The ICPD Programme of Action called for two-thirds of the annual cost to be borne by developing countries and the remaining one-third by donor nations like the United States. Using the agreed-upon ICPD burden-sharing rationale, donor nations would be expected to contribute one-third of the $12.1 billion total current cost—or $4.033 billion.
The most equitable formula for allocating the relative shares of the $4.033 billion contribution to meeting the $12.1 billion annual cost among donor countries should be based on each nation’s wealth relative to each other. The membership of the Development Assistance Committee (DAC) of the Organization for Economic Cooperation and Development (OECD) is composed of all the major industrial nations that provide official development assistance (ODA) to poor countries, amounting to $145 billion in 2016. Gross National Income (GNI) is the internationally accepted indicator for measuring national wealth. Under this measure, the U.S. economy represented over 41 percent of total donor nation GNI in 2016, the latest year available—U.S. GNI of $18.5 trillion divided by total OECD-DAC GNI of $44.9 trillion.
The final computation produces a recommendation of $1.66 billion for fiscal year (FY) 2020 as the appropriate U.S. share of the total annual funding from all sources required to meet the current unmet need for modern contraception of 214 million women in developing countries—41.16 percent of $4.033 billion. Embedded within the $1.66 billion target is an allocation of $111 million for a U.S. contribution to the United Nations Population Fund (UNFPA), the only intergovernmental institution with an explicit mandate to address the reproductive health needs of women and men worldwide.
To put the size of the recommendation in perspective, if $1.66 billion were to be appropriated by Congress for FY 2020, that level of spending would require a near tripling (2.7 times) of the current FY 2018 enacted level of $607.5 million. Given the current political and budgetary environment, approval of such a dramatic increase in funding for USG international FP/RH programs is completely unrealistic as appropriated levels have plateaued at just over $600 million for the last eight fiscal years. Further complicating the political and fiscal reality, the Trump-Pence administration’s first two budget requests have proposed zeroing out funding entirely or cutting in half the prior year enacted level, respectively. However, the historic record for highest congressional appropriations for USG overseas FP/RH programs in constant dollars, set in FY 1995, would amount to nearly a billion dollars today—$975 million—when adjusted for inflation.
Strategic investments in sexual and reproductive health saves lives. The Guttmacher Institute’s analysis found that meeting the current unmet need for modern contraception in developing countries would result in a decline of approximately three-quarters in “unintended pregnancies (from the current 89 million to 22 million per year), unplanned births (from 30 million to seven million per year) and induced abortions (from 48 million to 12 million per year).” In addition, for every additional $1 spent on contraceptive care, $2.20 is saved on maternal and newborn care because of declines in the number of unintended pregnancies.
Perennially, family planning advocates are confronted over the massive size of the funding “ask” for FP/RH programs with suggestions that it won’t “pass the laugh test” when presented to congressional appropriators and executive branch budget staff. The fact is that the FP/RH price tag is not summarily dismissed by policymakers and is routinely pointed to as a model for other health and development sectors to emulate.
The key players in the budget and appropriations process understand it for what it is—a calculation of the appropriate U.S. share of the global investment required to satisfy the current unmet need for modern contraception of women in developing countries, derived from a methodologically sound estimate of the total annual cost to achieve that goal and based on a reasonable burden-sharing rationale for contributions to the effort by donor and developing countries. Nothing more and nothing less.
Everyone involved understands that Congress is not going to enact a near tripling of FP/RH funding in the final appropriations bill anytime soon. But the funding recommendation helps inform policymakers’ priority-setting and decision-making by providing a solid, evidence-based estimate of what the U.S. government should be investing in contraceptive availability and use—even if it doesn’t.
We are fighting back against the onslaught of harmful policies that discard reproductive rights.
Stay informed about the issues impacting sexual and reproductive health and rights.
